Vaginal yeast infection. Three dreaded words for women everywhere. Seriously, I cringe at the thought!
The truth is it is estimated that nearly 75% of women in the US will have had at least one yeast infection in their lifetime!
So it is likely that you, too, have suffered from these opportunistic critters (or that you WILL!)
As an Emory University trained board-certified Gynecologist and Obstetrician, and an expert in women’s health and sexual health, I have treated thousands of women over the years.
Missy, 29, PCOS And Recurrent Yeast Infections

I remember Missy, who came in with her third yeast infection in a year and I’d already treated her with Diflucan twice. So I sat her down and told her we have to get to the bottom of this and heal her gut and vagina by stopping sugar, increasing greens and healthy fats (Keto-Green® diet philosophy) and I instructed her to begin a probiotic and Mighty Maca® Plus.
Well… she was LIVID. All she wanted was a pill and quick fix (which I did prescribe her). However, when she humbly showed up with her fourth infection three months later she was ready to do anything — those of you who have suffered from yeast get this — me too! Once following those diet and lifestyle changes she did finally heal from recurrent yeast infections, and she also lost 20 lbs, felt better than ever and conceived a little boy after two years of trying!
See, get to the root cause and make lifestyle changes to improve your life for the better!
Casey, 49, Constant Vaginal Discomfort And Irritation

There was also Casey who had constant itching and vaginal irritation but no discharge. I’d treated her with anti-fungal, cultured her vaginal secretions and found negative growth; even used gentian violet to no avail. I used my Nancy Drew mentality and determined it was a combination of food sensitivities and latex condoms. Once we corrected those she was back to normal healthy comfort. So, again getting to the root cause, makes all the difference!
Ok, I can’t resist one more example, but I trust these are really helpful!
Sandy, 62, Professional Golfer, Recurrent Aggravating Yeast Infections For Years

Sandy who was suffering from recurrent vaginal yeast infections started using and she had immediate fabulous results as she was suffering from severe vaginal atrophy as a breast cancer survivor.
After two weeks she had improved moisture but started to get a yeast infection again.
Now, when you go from the "Sahara" to the "Amazon", so to speak, yeastiest thrive. I instructed her to continue the Julva® but to add a topical anti-fungal plus Diflucan 200mg per day x 5 days (because also as a golfer in the heat and sweating we had to be aggressive). I also added an oral probiotic. No women should suffer from vaginal yeast!
Julva® improved her vaginal tissue and pH and after that initial treatment, she has not had any other vaginal itching or yeast! (And her golf game is even better!)
3 different scenarios and a comprehensive approach solved the problem!
So Now, Let’s Talk About Vaginal Yeast — Even Though We Don’t Want To!
Keeping women and vaginas healthy and happy has been my mission!
Providing natural treatment methods supporting infertility challenges, pregnancies, vaginal atrophy miseries (vaginal dryness, incontinence, pain and libido issues), perimenopause and menopause hormone decline… and through all of these ages and stages, vaginal yeast infections consistently rank at the top of the feminine issues women address.
They are also one of the issues that women can affect and help prevent — and also often self-treat.
In this article, I’ll be talking about all things vaginal yeast infection. I’ll talk about a few other “V” issues as well.
Much of the content of this piece came out of a wonderful (and fun!) interview I did with a great friend and peer, Dr. Mikell Suzanne Parsons, a functional chiropractor who does put the "Fun" in functional.
In this article, you’ll learn:
- What’s “normal” down there (and yes, discharge and bacteria are normal!)
- Smells may not be normal… (but the V is self-cleaning!)
- What is this bugger called yeast?
- Things that can affect our getting a yeast infection (it’s all about hormones, ladies!)
- Why our gut health is important to our V!
- Preventative steps you can take
- Self-treating for yeast infections
- When to call your doc — and why yeast infections are important even if you aren’t sexually active!
- Other vaginal problems to be aware of
What’s “Normal” Down There (And Yes, Discharge And Bacteria Are Normal!)
Yes, discharge is normal. And what’s “normal” is unique to each of us and also fluctuates if we are still ovulating.
Typical “normal” discharge is clear to pale white, or creamy.
For women who are pre-menopausal, it is normal to have about one-half to one teaspoon of discharge daily. We have glands within our vagina that constantly secret fluid, as well as the lining of the vagina, which is called the mucosal layer, and is made to be kept moist like the inside of our mouth. Our body is constantly shedding cells from our cervix, vagina, vulva and surrounding areas. This shedding is under the control of estrogen, so women who are menopausal normally have less discharge for this reason.
When we ovulate our discharge can become thicker, stringy… it looks like it has some elasticity to it. This is all about our hormones, ovulation and our fertility! This thicker discharge is completely normal and called the spinnbarkeit.
Having Bacteria Is Also Normal!
A woman’s vagina typically has a lot of “good” bacteria in place which thrives in the vagina’s low, acidic pH environment. A healthy vagina is usually between 3.5 and 4.5 in terms of pH. You can actually test that using a pH test strip; just hold a test strip at the mouth of your vagina in contact with the secretions.
The main bacteria found in the vagina is from the Lactobacillus species, the most common of which are L. iners, L. crispatus, L. gasseri, L. jenesenii; followed by L. acidophilus, L. fermentum, L. plantarum, L. brevis, L. casei, L. vaginalis, L. delbrueckii, L. salivarius, L. reuteri, and L. rhamnosus.
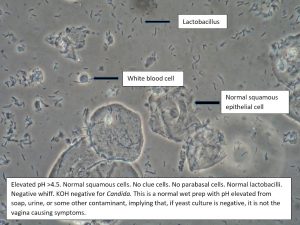
Normal vagina wet prep (courtesy)

When the vagina gets more alkaline, other bacterial infections can occur. I’ll talk more about this in a moment.
Often we see these pH imbalances happen at times of hormone fluctuations (menstruation, pregnancy, stress, underlying disease such as diabetes, menopause, etc.)
Smells May Not Be Normal… (But The V Is Self-Cleaning!)
The vagina has a natural body odor that shouldn’t smell fishy or overly sweet. Many women obsess about this but needn’t.
A fishy odor likely means a bacterial infection called, “bacterial vaginosis”. A sweet odor may indicate a yeast infection.
Every woman is different so you need to be aware of what’s “typical” for you in terms of smell. It can also be affected by your diet.
An odor can indicate an imbalance in pH or an infection. For example, women may experience a fishy odor and perhaps some discharge after sex. What happens is that a man’s sperm and seminal fluid are alkaline. With the alkalinity introduced into the vagina, any established (bad) bacteria may start to thrive. For this reason, I usually suggest women simply bath within 24 hours of having intercourse, with no soap or use of other chemical irritants, please!
The V Is Naturally Self-Cleaning (Please Don’t Douche With A Few Exceptions)
The vagina is naturally very self-cleaning so I seldom recommend douching as that disturbs the healthy pH and can kill good bacteria (often referred to as the healthy flora).
Would you believe women were historically told to douche with Lysol?! It’s true!
See this shocking ad!
If secretions become colored (yellow, grey, green can point to an infection), bloody or smelly, you should discuss with your doctor — not douche — and I get into more detail below!
If the smell is particularly troublesome — after you’ve ruled out other issues with your doc — you can make a vaginal douche (this is the only time I recommend douching) by dissolving a probiotic capsule in a little-filtered water. I’d use at least 50 billion multi-strains of good bacteria.
Some of my patients have used probiotics dissolved in yogurt and insert that (assuming you don’t have any type of dairy intolerance) into their vaginas.
Also, see my DIY recipe with essential oils below.
What Is This Bugger Called Yeast?
If you experience a thick white cottage cheese discharge and/or a sweet odor you likely have a yeast or Candida infection.
Candidiasis is a fungal infection (not a bacterial infection) caused by yeasts. There are many types or species of Candida yeasts found in humans but the most common is Candida albicans.
A lot of people hear the word Candida and think about yeast overgrowth issues in the intestinal tract or gut. You may also have heard of thrush, which is candidiasis that develops in the throat or mouth.
Candidiasis can also occur in the vagina, where it is usually referred to as a “yeast infection,” but could also be called, “candidal vaginitis”, “vulvovaginal candidiasis”, or “vaginal candidiasis.”
I actually talk about the vagina as being part of the gut, so keep that in mind. What’s good for the gut is good for your vagina, and vice versa!
So just like sugar, alcohol and other white and processed carbs aren’t good for supporting your gut microbiome, they aren’t good for your vagina, either!

A lot of us have candida in our bodies, and it can live there without causing any problems. It is an opportunistic type of organism, meaning yeast can hang out and just patiently wait for the environment to become more hospitable to their ability to multiply and thrive. It has been estimated that some 20% of all women normally have candida in the vagina without having any adverse symptoms.
The problem is when there are hormone changes, changes in the immune system or other factors (use of antibiotics is a very common culprit) that change the vagina in a way that encourages candida to multiply.
Yeast infections are common in the US and when I had my practice it was a very typical complaint, especially with my pregnant patients. Yeast infections are the second most common complaint about abnormal vaginal discharge, after bacterial infections.
Symptoms of yeast infections can include:
- Cottage cheese-like discharge (common, but some women may not have this)
- Vaginal itching or soreness
- Discomfort or pain when urinating
- Discomfort or pain during sexual intercourse
What your doctor may see:
- Redness of the vaginal walls
- Swelling or cracking of the vaginal walls
- Thick white discharge
- Sweetish odor with low pH
- A wet prep or vaginal smear under the microscope that shows fungi (see the photon above)
Things That Can Affect Us Getting A Yeast Infection (It’s All About Hormones, Ladies!)
The vagina has many hormone sensitive receptors, which is why a woman’s risk of getting a yeast infection increases during times of hormone fluctuations.
Periods associated with high estrogen levels, in particular, provide an enhanced feeding ground for yeast due to an increase in glycogen production, which yeast will thrive on. Low levels of estrogen can cause problems, too!
Yeast infections are more common during:
- Menstruation/ovulation
- Pregnancy
- Use of oral contraceptives (especially high estrogen variety)
- The transition to peri-menopause and menopause (decreased estrogen is tied to a decrease in lactobacilli and more susceptibility to infections, as well as thinning and drying)
- Times where poor lifestyle factors affect gut health and hormone balance: when stressed, experiencing environmental toxins, lack of sleep, poor diet, poor digestive health or a weakened immune system
- Times of having uncontrolled blood sugar issues and insulin levels while having diabetes
- Times of sexual activity (after sexual intercourse)
- Menopause when going from dryness to increased lubrication with hormones or creams
And also can occur when the vagina’s healthy flora is compromised:
- Using douches or chemical/perfumed vaginal products (kills off the good guys, too!)
- Using medications such as antibiotics or steroids (kills the good guys, too!)
- Some spermicides can cause irritation and pH imbalances; some condoms such as latex
Why Our Gut Health Is Important To Our V!
I consider the vagina to be part of our body’s gastrointestinal tract (GI tract or gut). It is important to get things healthy there in order to get things healthy in your vagina. An alkaline diet is most supportive of overall health.
So you are likely saying, but isn’t alkaline bad for the vagina?
Yes, different parts of the body have their own unique pH. The vagina is healthiest as an acidic environment. But your body’s overall net pH is alkaline for greatest overall health. An alkaline diet will support a healthy gut and vaginal microbiome.
Along with an alkaline diet, the best way to keep the GI tract and your vagina healthy is to take a good daily probiotic. Orally is fine. Lactobacillus and Bifidobacterium are the probiotics that are most commonly used for vaginal health. You can also purchase probiotics that are inserted vaginally or even make your own.
Diet and lifestyle important to your gut health (digestion, detox, and immunity) are also relevant to the vagina. In all of my women’s restorative health programs, we follow a Keto-Green® Diet for this reason.

Eating too much carbs and sugars allow yeast to thrive throughout your body. That includes most artificial sweeteners as well (except Stevia and Xylitol). I love Xylitol as it has been shown to have almost an anti-fungal capability relating to candida.
Food sensitivities can also come into play. You might wonder how that is possible, that what you eat — and have issues with — can’t possibly impact your V!
But again remember that the vagina is essentially an extension of the gut (according to Dr. Anna!) so anything that affects one has the potential to affect the other.
Preventative Steps You Can Take
Along with eating a Keto-Alkaline diet which focuses on the avoidance of foods such as sugar and carbs (and removes common food sensitivities) that yeast love and need to thrive, increasing your healthy dietary fats via taking in more Omega 3s is also helpful.
A diet rich in olive oil, coconut oil, nuts, olives, and avocados is great nutrition and good fats for our cell membranes too. Again, I also recommend a daily probiotic.
When on antibiotics, it is especially important to take probiotics during treatment or soon after. You might consider vaginally inserted probiotics if you have a history of yeast infections.
Hygiene Matters!
There are also many “hygiene” things you should do, such as avoiding keeping your V in a moist condition for an extended period of time, such as sitting around in sweaty gym clothes or a wet bathing suit.
And tight clothes and/or wearing materials that don’t breathe are also a no-no.
Check out your laundry detergent (that you are washing your panties in!). Are there perfumes and chemicals that could be causing a problem?
Women’s sanitary products can sometimes be culprits. Tampon trauma can occur, and some sanitary products contain bleaches, perfumes or other chemicals. Read labels and consider a non-toxic option such as Lotus Liners.
Should you begin to feel “off”, there are things you can do to self-treat the problem. I do suggest that you only attempt this for about a week, though.

Self-Treating For Yeast Infections
You can self-treat yeast infections with Over-The-Counter (OTC) treatments such as Monistat, terconazole or herbal preparations, apple cider vinegar with water or probiotic douche; but check in with your doctor should you have recurring infections because it could be a reflection of something going on elsewhere with your digestive or gastrointestinal tract or another problem.
My favorite DIY Vaginal Yeast treatment:
- Warm coconut oil to liquid – 4 oz
- Add essential oils – 3-5 drops tea tree oil, thieves, and lavender (or rose) oils. (Other essential oil options are the oil of oregano and myrrh)
- Mix together well
- Massage warm mixture on to external vulvar area — and gently to vaginal tissue — if it is too strong as indicated by irritation or burning feeling, dilute with more coconut oil
- Pour remaining mixture into small ice cube trays and freeze
- You’ve now created your own vaginal suppositories to use twice daily —you may need to use for 7-10 days
- To make it stronger you could add 1 tbsp of boric acid to the mixture if needed
If you have another condition you are being treated for, such as diabetes or pregnancy, you’ll also want to discuss any self-treatment options with your physician. As well, if you are in any kind of pain or if there is any bleeding or no improvement in self-care in 3 days.
If you don’t see any relief, or you get recurrent infections, you should go to your doctor and ask for a culture to determine the specific DNA strand that needs to be dealt with. Each type of DNA requires different medications to best eradicate it! Even if you want to deal with your yeast infection “naturally” (through diet, etc.) don't let the yeast infection linger on. Use medication and get rid of it so it won’t cause additional inflammation and potential new issues.
A Few More Self-Treatments You Can Try Include:
- Probiotics, inserted vaginally (either using probiotic yogurt or even a capsule)
- Make a garlic tampon! Yes, really! Take a clove and tie a strong/long string around it and insert it during the day. Take that out and insert an opened probiotic capsule at night. Do that for a few days
- Oil of oregano – a great antifungal, I suggest an oral dose daily; some people recommend douching with it as well
- Essential oils – in a 2016 study several essential oils, such as mint, lavender, tea tree oil, oregano, winter savory and basil were used on candida — this was compared to antifungal drugs that are commonly used for vaginal yeast infections (clotrimazole, itraconazole, and fluconazole). These essential oils inhibited both the growth and the activity of Candida albicans more efficiently than clotrimazole.
- No vaginal intercourse – give things a rest down there! Enjoy other pleasures!
- Boric Acid capsules – this is prescription but is something I commonly used to treat my patients. Boric acid has antibacterial properties and is great as an antifungal. Studies have shown it to be very effective against Candida. I routinely prescribed 600mg capsules to be inserted vaginally twice a day for 10 to 14 days.
- Caprylic Acid – also contains antibacterial and antifungal properties. Take this orally to help naturally address yeast growth in the gut.
- Coconut oil – one of the reasons I used coconut oil in my women’s restorative cream for the vulva, Julva, is for its natural anti-fungal properties! There are studies that show coconut can reduce Candida albicans infections.
When To Call Your Doc And Why Yeast Infections Are Important Even If You Aren’t Sexually Active
As stated above, after one week of self-treatment! Or if infections are recurring or if there is discomfort or pain.
Note that yeast infections are frequently self-diagnosed incorrectly (meaning the issue is something else).
After a week you may need to get a culture to determine the specific DNA strand so can kill it. You may even need a biopsy.
If your doctor doesn’t want to do a culture you can ask your local compounding pharmacist for a more holistic doc or check out the IFM link for finding a functional medicine practitioner in your area.
Remember, having a vaginal yeast infection isn’t just about sex, it is about vaginal — and your overall — health.
Things can get worse, besides being uncomfortable. Vaginal health is also about things like preventing incontinence, and cancer detection (so get a Pap Smear!!) and if candida is bothering your vagina it is likely overgrown in your gut which can cause leaky gut and other health issues. So you really do need to see a doctor who will likely prescribe something for you as well as have you continue to work on preventative measures.
Prescription medications include:
- Diflucan – very commonly used oral prescription
- Terazol 3 vaginal prep
- Monistat-1 or -3
- Nystatin oral and suppositories
Other Vaginal Infections To Be Aware Of!
There are many infections that can occur in the vagina, sexually transmitted diseases and otherwise. You can find a lot of information on the internet on all of these. The CDC provides good summaries of each of them, including symptoms to watch for, how a diagnosis will be made and what treatment options are available.
Discharge that indicates an infectious nature includes:
- Yellow discharge can indicate bacteria, atrophic vaginitis, chlamydia. A frothy and blood-tinged discharge can indicate trichomonas. It should always be evaluated right away by your physician.
- A greenish discharge is classically associated with gonorrhea which needs treatment right away.
- These can also cause itching so should not be confused with a yeast infection and that is why persistent symptoms must be evaluated by a wet prep and physical exam.
Here is a brief summary, taken from my “All Things V” e-book, on other vaginal infections to be aware of.
Bacterial Vaginosis (Gardnerella Vaginitis)
This is a very common cause for odor and discharge. As mentioned earlier this is caused by a change in the type of bacteria found in the vagina, often as a result of sexual intercourse. It may be self-treated.
Trichomoniasis
This is a very common sexually transmitted disease (STD) caused by a protozoan parasite called Trichomonas vaginalis. It can cause itching, burning, and soreness of the vagina. It can also cause discomfort with urination. A doctor needs to diagnose this infection and write a prescription for medication (metronidazole or tinidazole).
Chlamydia
Another common STD. In women, it can cause pelvic inflammatory disease (permanent damage to the reproductive system) and can affect a woman’s ability to later get pregnant. Some women won’t experience symptoms. If you are sexually active with different partners talk to your doctor about being tested. STDs are a great reason why you should use a condom!
Gonorrhea
Gonorrhea is often hard to detect as many women do not have obvious symptoms. Even when a woman does have symptoms, they can be easily mistaken for a vaginal or bladder infection. A woman may experience increased vaginal discharge, a burning sensation when urinating, and/or vaginal bleeding between periods.
Because it is difficult to detect it may not be treated. Untreated gonorrhea can cause serious and permanent health issues. Those issues include pelvic inflammatory disease, blocked fallopian tubes, ectopic pregnancies, infertility and long-term pelvic pain.
It can be treated, typically with intramuscular ceftriaxone and azithromycin. Note that treatment does not repair any permanent damage done by the disease! Another concern that I have is that antimicrobial resistance in gonorrhea is now occurring such that successful treatment of gonorrhea by traditional therapies is becoming more difficult.
HSV (Herpes Simplex Viruses)
Herpes simplex viruses can’t be cured. There are two types, oral herpes (also called herpes type 1, or HSV-1) and genital herpes (also referred to as herpes type 2 or HSV-2). Both cause sores around the infected areas (around the mouth in oral herpes and around the genitals in genital herpes). And the sores come and go; usually erupting due to some physical or emotional trigger. There are prescription medications available that can decrease the pain related to an outbreak as well as reduce healing time during an outbreak.
HPV
About 79 million Americans are currently infected with HPV and many people don’t know they are infected until they are diagnosed with other health problems such as cancers or genital warts. HPV is the most common STI. There are vaccines available to address the HPV infection prior to there being incremental health problems, however, I am not at all convinced that there are benefits that outweigh the potential harm.
Skin conditions — like lichen sclerosus
Many women ask me about lichen sclerosus (LS). It is interesting that LS has a bimodal age distribution. Typically it occurs at age 6 or around age 60, but we are seeing it in younger peri-menopausal women as well. It is associated with atrophy and 1-2 out of 100 menopausal women experience it. The current medical treatment is with using steroids such as clobetasol but it is often a chronic condition. Clinically, I have found that improving the vulvar hormonal health to improve the surrounding and deep tissue, improves this condition.
Lichen sclerosus causes intense itching around the vulvar tissues. The tissue is very itchy, tender and easily irritated (so obviously intimacy is often completely off the table).
As a gynecologist, I would state that lichen sclerosus is probably one of the most difficult conditions to treat.
If your doctor has diagnosed you with having LS, please talk to him/her about trying Julva. Julva users having LS have had good results. With LS you should consider starting Julva, though, at half the dose and on the healthier tissue surrounding the LS. This will allow some gentle nourishing of the delicate vulvar skin to start. This is a conservative approach as we’ve had many Julva users with LS start out with the full dose. Discuss with your doctor, and be patient… this may take a little longer. I offer a full 60-day money back guarantee if you do not see results.
Vulvodynia
Vulvodynia and Vulvar Vestibulitis Syndrome (VVS) — are pain disorders of the vulva. It can feel like a burning or cutting pain and can really disrupt a woman’s life. It affects up to 10-15% of women seeking GYN evaluations. There are many potential etiologies that range from auto-immunity, candidiasis, and sexually transmitted infections such as herpes or HSV, trauma, endometriosis, atrophy and more.
Here’s some additional info relating to that.
All of my lifestyle and nutrition recommendations can help to improve this condition. It is frustrating but patience and perseverance as well as getting to the root cause can help improve quality of life.
Women who experience vulvodynia suffer from chronic vulvar soreness, rawness, stinging or pain. The pain and discomfort are sometimes referred to as “unprovoked pain”, although activities that apply pressure to the vulva, such as sitting or even sexual intercourse, seem to exacerbate symptoms.
You can learn more about the condition at the National Vulvodynia Association.
I have heard some good feedback on the Vulval Pain Society so you might wish to check their resources.
Both these organizations provide info on the following condition, Vestibulodynia, as well.
Vestibulodynia (Vestibulitis)
This is a form of vulvodynia. The pain is specific to the tissue surrounding the vaginal opening, referred to as the vestibule. It is usually referred to as “provoked pain”, meaning, caused by some type of contact.
The vestibule is where the vulva meets with the vagina. It is extremely sensitive. Some women may even experience pain from clothing touching the area. Sex can be impossible.
The pain can occur part on your body that contains the Bartholin’s gland (which produces vaginal lubrication), the urethra (where you pass urine) and a number of the small minor vestibule glands which also produce vaginal discharge.
Vaginal dilators can be inserted to relax the muscles around the entrance to the vagina and to gently stretch the area. These can be helpful to overcome the tension in the pelvic floor muscles that can occur in vestibulodynia.
Final Words On “V” Health!
It does seem as if our vaginal health is quite fragile, but we also have to take into account the elements that might affect its natural state such as what we eat, what type of undergarments we wear, what we’re putting on our body etc.
But as long as we are willing to get to the root of the problem, we will find ways to solve them. Keeping things in a balanced state down there is one of the key ways we’re going to keep vaginal yeast infections at bay and keep you feeling fresh.
My Julva cream has helped well over a thousand women keep their lady bits moisturized, balanced and in shape. I urge you to consider my Julva restorative cream for the vulva trial pack and let me know how it goes for you. Just like my other patients, I promise you won’t regret it.
Please, ladies… take care of your vaginal health… pamper things down there!
With that in mind, I’d love for you to consider my Julva restorative cream for the vulva.