This is Part 2 of a 2 part series on hysterectomy.
In Part 1, “What You Need to Know About Having a Hysterectomy” I talked about why women have a hysterectomy and what some of the common side-effects can be (such as early onset menopause, incontinence, vaginal dryness, pelvic prolapse, chronic pain, low libido and more).
I also talked about the linkages between having a hysterectomy and having an increased risk for heart disease and dementia. Yet I do recognize that the advantages ideally are the resolution of the symptoms requiring surgery to begin with.
While a hysterectomy may be the best strategy for certain health scenarios such as cancer, most of the hysterectomies that occur today are not about cancer. These surgeries are performed most often for “benign conditions” (fibroids, bleeding, cramping, endometriosis, etc.) that can be quality-of-life affecting, but not life-threatening, and can be addressed in many cases by alternatives that don’t have the side-effects and risks that a hysterectomy does.
Please note that I am talking about these types of benign conditions relating to saying “no” to having a hysterectomy. And also note, always make decisions about your health in concert with the recommendations of your physician – who knows your own unique health status - versus relying on generic educational information posted on the internet.
A hysterectomy can be life saving and enhance the quality of life for many and I have performed many in my lifetime. What I worry about is it being a 1st resort vs. last resort. In fact, a mom recently wrote me about her 17 y.o. daughter requesting a hysterectomy for convenience… she hates her periods. This is heartbreaking to me.
In this article I’ll be talking about,
- Addressing the most common root cause, estrogen dominance
- Lifestyle interventions that can help avoid hysterectomy
- Uterine saving alternatives to hysterectomy for non-cancer-related conditions
- If you’ve already had a hysterectomy
First let’s talk about how best to support your body in avoiding hysterectomy by optimizing your health with natural remedies you can implement today. These natural strategies address the root causes that can result in unnecessary hysterectomies, in particular relating to estrogen dominance. In my clinical practice I saw that by focusing on these interventions many women will show significant symptoms improvement in 1-2 menstrual cycles or in about 6-8 weeks.
Then I’ll talk about uterine saving alternatives to having a hysterectomy, including the use of hormones.
Finally, I’ll end with a few thoughts relating to those already having had a hysterectomy (note that if you have already had a hysterectomy these same lifestyle interventions can likely help you!) as we know that if the root causes aren’t addressed many symptoms will linger with or without a uterus or ovaries.
Addressing the most common root cause, estrogen dominance
As I mentioned in Part 1, when I got to (and resolved) the root cause of many uterine issues I needed to perform 90% fewer surgeries! A hysterectomy doesn’t usually address the root cause of the problematic uterine condition you may be dealing with! In many cases, the root cause of the most common problems is something called estrogen dominance.
Estrogen dominance is often the underlying cause for women having fibroids, endometriosis, PMS, ovarian cysts, painful periods, and other issues relating to “benign” conditions often addressed via a hysterectomy. Estrogen dominance can occur due to having underlying conditions such as hypothyroidism or PCOS, as well as everyday impacts to hormone balance such as poor diet, stress, lack of sleep, environmental toxins, poor detoxification, and more.
Estrogen dominance is not only about the levels of natural hormones (estrogen, progesterone, cortisol, insulin, etc.) the body is producing, but is greatly influenced by outside hormone exposures (endocrine disruptors as an example) as well as your body’s ability to detox spent hormones. So having a poor detox/elimination system (due to poor diet, being a poor methylator, dehydration, etc.) can cause hormones such as estrogen to be recycled versus eliminated, which can become very toxic. (I discuss this in more detail in Chapter 7 of my book, The Hormone Fix).
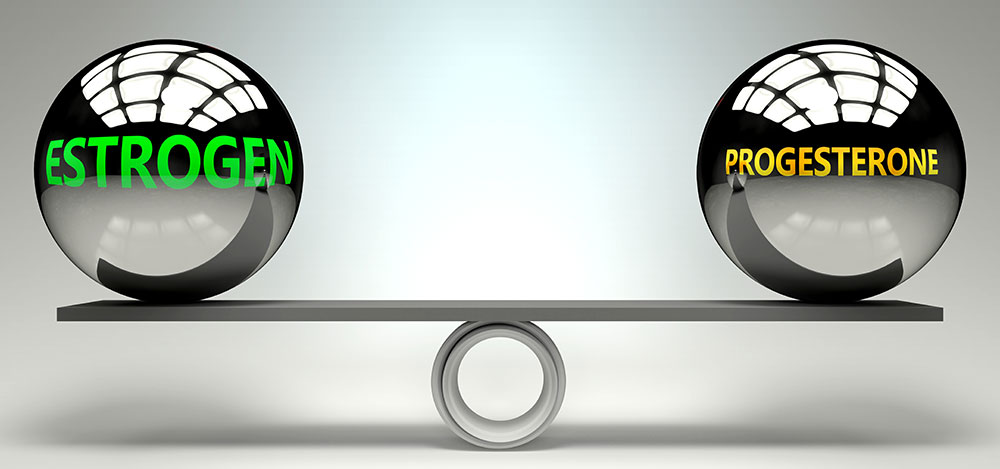
What a lot of women don’t understand is that this hormone imbalance isn’t just about “too much estrogen.” Estrogen dominance is the ratio of estrogen to progesterone. Even if a woman has low levels of estrogen she can still be estrogen dominant if she has even lower levels of progesterone.
A woman can have suboptimal levels of progesterone when she is in her child-bearing years, and it can impact her chances at becoming pregnant. This is called a Luteal Phase defect, but can be addressed by progesterone therapy. You can read a wonderful story about a 36 year old woman named Nikki who was experiencing fertility problems, and how progesterone therapy, as well as naturally supporting the adrenals, improved fertility and overall health (when we are under stress our bodies actually steal progesterone to make more of the stress hormone cortisol! So anything that supports the adrenals can help improve bioavailable progesterone).
During perimenopause, a woman’s hormones fluctuate due to declining estrogen and fewer ovulations, so less progesterone is also produced. This can result in heavy bleeding, irregular periods, break-through bleeding, spotting and the like.
During menopause (whether that be natural or surgery-induced), estrogen is minimally produced in the ovaries (although still made in small amounts elsewhere in the body). Progesterone levels drop significantly. I find that many still suffer from estrogen dominance symptoms. It is also a common co-occurrence with hypothyroidism.
So we really want to address issues relating to estrogen dominance as the root cause of uterine conditions. Other hormones also come into play, including cortisol and insulin. We’ll talk about how natural strategies can help with those.
Lifestyle interventions that can help avoid hysterectomy

How you live your life can affect,
- Whether you develop hormone imbalances that can contribute to uterine issues and other quality-of-life affecting symptoms
- Whether you can successfully and safely avoid a hysterectomy should you develop a uterine condition
- How you can heal and minimize side-effects should you undergo a hysterectomy or alternative medical surgery
- How healthfully you go INTO having a hysterectomy or alternative medical surgery. Yes, even if you decide to have a hysterectomy – assuming it isn’t an emergency – let’s focus on optimizing your hormones and your health PRIOR to having the procedure to ensure optimal results. I can tell you that I used to do a lot of procedures for prolapse, so prescribed bioidentical androgen hormones like testosterone and DHEA prior to the procedure to strengthen the vaginal musculature and improve its integrity…and low and behold, when the woman came in for a pre-operative consult, many no longer needed the surgery! This is actually why I created Julva...you can read the story here.
There are many lifestyle interventions that can help women with uterine health. Here are the ones that I strategically focus on for maximum results:
- Improve detoxification: Healthy detox is an important part of eating Keto-Green™. You can learn some of the basics by taking my free 10-day Breeze Through Menopause class. Or get on a modified elimination diet (removing common food sensitivities such as gluten and dairy), increase fiber, bump up omega-3 essential fatty acids, take a quality probiotic to improve gut health, and increase your movement! Digestion is important! Your body can’t absorb needed nutrients if your digestion is not optimally functioning! I have found that food sensitivities such as dairy are often a root issue relating to poor digestion and detox.
- Decrease estrogen intake (and increase elimination): Stay away from oral hormone replacement therapy and oral contraceptives. Eat organic, especially relating to eating hormone-free and antibiotic-free meats, poultry, and eggs. Reduce exposure to environmental toxins such as those found in your skin care products and kitchen (check out EWG.org for more info than you ever wanted to know about how everyday exposures to endocrine disruptors can increase your estrogen levels (your man’s, too!). I suggest detox support specifically focused on estrogen detoxification. My Zenful supplement blend of biologically active folate and other key methylation ingredients promotes estrogen detoxification and female hormone cycle balance.
- Consider bio-identical progesterone to also help balance estrogen in your body: Useful in supporting a regular menstruation, addressing infertility, and for symptom relief for menopause, including mood swings, sleep disturbances, hot flashes, etc. Restorative sleep helps support your brain in modulating healthy levels of key hormones. You will appreciate the improved mood as well! My Balance Cream is a wonderful formulation to try. Ask your doctor for a prescription for bio-identical progesterone such as Prometrium or cream.
- Improve insulin sensitivity and maintain a healthy weight (BMI is particularly important). A Keto-green diet will support your achieving the many benefits of alkalinity which includes normalizing insulin as well as your weight-loss goals. An unhealthy BMI and obesity increases your risk for prolapse, incontinence and other uterine issues and also impacts your risks for many other diseases, including insulin resistance, pre-diabetes and Type 2 diabetes.
- Tame the cortisol tiger and manage that stress (and add more fun into your life)! When we are stressed out our body attempts to produce greater levels of our stress hormone cortisol. And guess what…when it can’t keep up the production levels it starts to steal from other hormones, and one of the hormones it steals from is progesterone! Your stressed out adrenals will take progesterone to make more cortisol, often resulting in estrogen dominance and all of the symptoms we’ve been talking about. One of the best ways to reduce cortisol is to focus on better stress management; try HeartMath, yoga or meditation. Read chapter 8 in my book, “The Hormone Fix,” to learn more about how to stop stress from stressing you out! I like taking a walk in nature which also gives me good doses of vitamin D and oxytocin as well. Oxytocin is our hormone of love and bonding and can help counterbalance cortisol! Hug your pet, hold hands with your partner, or have an orgasm! All produce oxytocin! The uterus contains oxytocin receptors as well; there, oxytocin starts labor contractions and later is involved in milk production for breastfeeding. Another important strategy is diet! Research tells us that eating an acid heavy diet (sugars, carbs and processed foods) elevates cortisol, another reason for going Keto-Green. (1)
- Take adrenal adaptogens. Adaptogens help our body deal with its stress response. My favorite adrenal adaptogen is maca. Maca also is seemingly able to regulate estrogen levels without being hormone stimulating or estrogenic (learn more at the linked article). As a bonus it supports improved fertility! I love maca and have used it as a cornerstone nutrient and adrenal adaptogen in my Keto-Green Mighty Maca® Plus green superfoods drink. It contains organic kosher maca plus over 30 additional superfoods.
- Focus on pelvic health: So many women are now experiencing issues relating to prolapse and incontinence, as well as issues relating to vaginal dryness, pain and sexual function. There are lots of things women can do to prevent these issues or resolve them. Kegel exercises: can strengthen our pelvic floor muscles and improve all of these symptoms. Learn more about doing them correctly as well as other ways to improve your pelvic floor health here. You might benefit from talking to a pelvic floor therapist as well to learn about additional exercises and therapies.
- Add key nutrient support: multi-vitamin with minerals and iron
- Use locally applied DHEA to address common menopause symptoms (vaginal dryness, pain during intercourse, leaking and low libido) even prior to menopause (or after having a surgical procedure such as a hysterectomy). My beautiful over the counter Julva® cosmetic cream for the vulva contains restorative moisturizing ingredients and plant stem cells to help support the delicate tissue and mucous membranes around the urethra, vagina and rectum. It also contains DHEA, which our bodies naturally produce (but that declines with age). Women trying Julva have reported reduced issues with vaginal dryness, leaking and discomfort. Read one woman’s beautiful story about the benefits that Julva brought to her (and her husband, too!).
- Test, don’t guess! This is my mantra for best health! Testing provides you information that is important for you to make the best decisions to optimize your health. For optimal gynecological health I suggest:
- Annual pelvic exams and honest discussion with your doctor about root causes and alternatives should something be found
- Recommended hormone lab testing which includes thyroid testing, which can often be a culprit. This panel also includes a cortisol biomarker. You want your doctor to monitor all of these important markers as you make adjustments to diet, lifestyle, and/or hormones, so they’ll want to follow-up on these.
- Know your cortisol and insulin numbers; they are both major hormones which can greatly influence our health.
- Daily pH testing to monitor for alkalinity using urine test strips
- I am liberal in recommending pelvic/vaginal ultrasounds. Discuss with your doctor.
And know that even when you do everything right you may still encounter symptoms.
Sometimes these may be mild enough you can watch and wait, and have your physician monitor the situation (sometimes fibroids shrink after menopause, so depending on how long of a wait that is for a given woman – and what symptoms she has – watchful waiting can sometimes work). A lot more women have fibroids than women experiencing symptoms have fibroids! Many ovarian cysts are low risk for malignancy and can be monitored using ultrasonography. Endometrial issues can be seen in pelvic ultrasounds, etc.
In other cases, there are options such as the use of hormone therapies as well as medical procedures (other than hysterectomy).
Uterine saving alternatives to hysterectomy for non-cancer-related conditions

The problem with a hysterectomy is that it is really “One size fits all.” Sure, there are different types of procedures and a surgeon may opt to take out more organs than just the uterus, or just part of the uterus. But the outcome is really somewhat, “One size fits all.” A woman can no longer conceive, she’ll most likely go into premature menopause if she is premenopausal, and she is probably going to experience at least some side-effects related to ongoing hormone imbalance as well as the physical changes to her pelvic region.
The good news? Considering fibroids and abnormal uterine bleeding account for about five times as many hysterectomies as all gynecological cancers combined, they are also the two conditions which there are the most alternative treatments available (beyond hysterectomy)!
Hormone therapy
Along with any hormone medication I may recommend I still stress a woman address the lifestyle interventions just discussed. We want to optimize our overall hormone health!
Over the years I have found that bio-identical hormones including progesterone, testosterone and DHEA can make all the difference to women and their private parts, without concerns relating to cancer! Most of these are compounded through a pharmacy and require your physician to prescribe (which is good, as you should continue to have your hormone levels monitored).
Throughout all of my experience treating women I have also found that my Balance cream can be helpful in balancing out symptoms, both alone or even along with a progestin IUD, oral contraceptives and post hysterectomy.
Other hormones or medications that your doctor might discuss with you that are more prone to side-effects (than bio-identical hormones):
- Contraceptive medications and long-acting progestational agents (Implanon or Depo-Provera) – I don’t really like these options as I feel they introduce other issues. If we don’t need them for contraception it is best not to use them. Research has found that using contraceptive steroids to address bleeding and pain often still results in surgery requirements.
- Antifibrinolytic medication such as Tranexamic acid (Lysteda) was only recently approved for use in the United States by the Food and Drug Administration (FDA) but has been used in other countries for years. Tranexamic acid is an oral agent that slows excessive menstrual bleeding.
- Gonadotropin-releasing hormone (GnRH) agonists are effective therapy for women with fibroids who experience bleeding symptoms; the lead to amenorrhea in most women and provide a 35-65% reduction in fibroid volume relatively quickly. The drugs have significant side-effects so are best used short-term for pre-operative therapy (to reduce fibroid size, for example).
- Aromatase Inhibitors – can also reduce fibroid size and have fewer side effects than GnRH agonists.
- Progesterone Modulators (Mifepristone) – for controlling fibroid symptoms and size.
Uterine saving medical interventions!
For pelvic relaxation or uterine prolapse:
- Bio-identical vaginal testosterone/DHEA – work with a good functional medicine doctor and consider if vaginal testosterone/DHEA could be beneficial for your condition. I found it worked wonders for patients having pelvic prolapse, incontinence and many other concerns. Even if you end up needing a surgical procedure your tissue will be in much better condition.
- Pelvic strengthening: Kegel exercises as well as using Lelo balls can strengthen the pelvic floor. Kegels are the easiest way to both prevent and treat weakened pelvic muscles and associated prolapse. Just do them right! (check out my video at the linked page)
- Anterior and posterior repair - used to tighten the support tissues that hold pelvic organs in place, restoring their normal position and function.
- Paravaginal repair - used to attach the bladder and urethra to their normal position by attaching them to the pelvic side-walls.
- Suspension operation - a procedure that can lift and reattach organs including the uterus, bladder or rectum.
- Sacral colpopexy – uses a synthetic mesh, surgically implanted, to support the vagina after pelvic organ prolapse. Note that surgery through the vagina had been an option in the past but the FDA recently banned transvaginal repair. The surgery is now only performed via the abdomen. Surgical mesh is also used to address stress urinary incontinence, known as a mid-urethral mesh sling surgery. Listen to a helpful podcast I recently did with Dr. Betsy Greenleaf about incontinence therapies.
- Vaginal pessary - a pessary looks like a diaphragm and is inserted into the vagina to hold the uterus in place. Not ideal for longterm; preferred for when a woman is not a good surgical candidate.
For endometriosis or pelvic pain:
- Bio-identical hormone vaginal therapy
- Low-dose progestin intrauterine devices (IUDs, including Mirena, Skyla, Liletta, and Kyleena). These are birth control IUD medications, still systemic (meaning the hormones travel through the blood system and don’t remain local in the uterus) but with low circulating levels compared to oral hormone therapy (birth control pills) and they don’t contain estrogen; they are a reasonable alternative to the choice of otherwise having a hysterectomy! They address heavy bleeding and cramping related to fibroids and endometriosis. They are easily reversible. (Note: Paragard is another birth control IUD that contains no hormones, but it has no effect on symptoms such as heavy bleeding, pain and cramping.)
- Laparoscopic surgery to treat endometriosis: can remove growths or scar tissue relating to endometriosis while preserving the uterus and ovaries (and the ability to get pregnant). Still need to get to the root cause however!
For heavy bleeding or symptomatic fibroids:
- Bio-identical progesterone
- Low-dose progestin intrauterine devices (see above)
- Dilation and curettage (D & C) to address noncancerous growths or uterine lining issues such as bleeding: removes the lining of the uterus; can be used in situations where the lining has become too thick, has excessive bleeding or noncancerous growths or polyps on it. Keeps the uterus intact and a woman can still get pregnant.
- Endometrial ablation to address bleeding: the uterus lining is frozen, heated or microwaved to destroy it in order to stop heavy or long-term vaginal bleeding. A woman cannot become pregnant after this procedure.
- Uterine artery embolization for bleeding, pain and pressure associated with fibroids: less invasive than a hysterectomy and has definitely become a preferred alternative. This procedure is performed by radiologists, with the uterine arteries embolized (which means the blood vessels of the fibroids are blocked, causing the fibroids to shrink). Pregnancy is not recommended after this procedure and a noted side-effect is early menopause, but the uterus and other organs remain intact. Up to 30% of women who have this procedure done need to have the procedure repeated within the following 2 years, and have a hysterectomy within 5 years after having the procedure. But about two thirds of patients avoid a hysterectomy. Studies done on health-related quality of life 10 years after the procedure are similar to hysterectomy. (2)
- Magnetic resonance-guided focused ultrasound surgery is the newest treatment alternative for fibroids, approved by the FDA in 2004. This is focused ultrasound surgery that can be used to destroy individual fibroids, most often in an outpatient capacity. Women can still become pregnant and the treatment appears to offer long-term preservation of ovarian function.
- Myomectomy for fibroid removal without removing the uterus. There are a variety of methods that can be used (abdominal, laparoscopic, hysteroscopic). If your physician recommends this surgery ask if a power morcellator will be used as the FDA has warned against this for most women. While the outcome of myomectomy is similar to hysterectomy relating to symptoms resolution there can be an issue of fibroid recurrence.
- Myolysis: a procedure to shrink fibroids, often done laparoscopically the surgeon shrinks fibroids by heating them. You can still get pregnant after this procedure..
One additional comment about removal of the ovaries. I’ve seen statistics that show the significant impact associated with the removal of ovaries relating to the increased prevalence of heart disease and strokes, hundreds of thousands of deaths per year. Compare that to the fact that ovarian cancer is still relatively rare, with deaths in the low tens of thousands (for example, in 2015, according to the Centers for Disease Control and Prevention/CDC, there were 13,920 deaths in the US due to ovarian cancer).
Just be sure to discuss your own medical history and risks (for both cancer and heart disease, based on lifestyle, medical condition and genetic information you have!) with your physician prior to removing your ovaries. We don’t want to do this strictly out of fear.
If you’ve already had a hysterectomy

All of the earlier lifestyle interventions are still good advice. We know that symptoms often linger or can develop even after the uterus and/or ovaries are removed. Again we need to focus on addressing the root causes.
Note that I get a lot of questions from women who no longer have a uterus, and let me just say that even without a uterus you still need to balance your hormones, including taking progesterone if your symptoms warrant it. Progesterone is supportive of brain, bone and breast health; we really need it with or without a uterus! I routinely recommend my progesterone/pregnenolone based Balance cream to women even after they have a hysterectomy for symptom relief. It will help balance estrogen issues, even if a woman’s estrogen levels have declined.
Julva can also be helpful whether or not you have a uterus in addressing symptoms such as vaginal dryness and incontinence concerns.
Even without a uterus you want to continue to have annual exams and monitor your pelvic health. If you’ve had a hysterectomy you also want to be particularly watchful for common side-effects (pelvic prolapse, etc.) and risk factors (cardiovascular health).
If you have had an alternative surgical procedure to a hysterectomy make sure your surgeon provides information and an ongoing plan for postoperative followup relating to long-term effects and signs to watch out for (that may indicate the need for a repeat procedure or other intervention).
Let me know how you do.
Join me on Facebook as well, I have a special Keto-Green community where you can learn so much helpful information from wonderful women who have been working through their own health issues and seeing amazing results. While I can’t provide you with specific medical advice online (since we unfortunately don’t have a physician-patient relationship) I will provide as much information as I can to help you in advocating for your best health.
I want to empower each of you in your health for your entire lives and that’s why I wrote, The Hormone Fix! So many testimonials of improved menstrual cycles, fertility and menopausal symptoms are repeated to me, really daily.
Know that it’s never too late.
One of my favorite things to have in my pantry at all times are nuts and seeds, especially sesame seeds. They’re a nutritious source of plant protein with a laundry list of health benefits. My Sesame Seed Chicken Salad Recipe is a delicious combination of fresh and crunchy ingredients, resulting in one of my favorite light and refreshing salads!
Sesame Seed Chicken Salad

Ingredients:
- 3 organic or pasture-raised boneless, skinless chicken breasts (about 2 pounds)
- Zest and juice of 1 lemon
- 1/2 cup mayonnaise
- 1/3 cup sour cream or Greek yogurt (optional)
- 1 tablespoon Dijon mustard
- 1 stalk celery, chopped
- 1/2 cup pecans, almonds, or walnuts, chopped and toasted
- 1/4 cup chopped fresh chives
- 1 1/2 tablespoons sesame seeds
- 1/2 cup dried apricots, chopped (optional)
Directions:
- Brine chicken if desired (optional): Make bringing liquid by dissolving 1/4 cup salt into 1 quart of water. Place chicken breasts in brine for 15–30 minutes.
- Remove from brine and pat dry. Discard brine.
- Cover chicken with cold water in a deep skillet or medium-size pot and add 1 teaspoon salt. Bring to a boil over high heat, then reduce the heat to medium-low and simmer, uncovered, until the chicken is cooked through, about 15 minutes. Remove the chicken and let cool.
- Place lemon zest and juice into a large bowl. Stir in the mayonnaise, sour cream, mustard, celery, nuts, chives, sesame seeds, ½ teaspoon salt, and pepper to taste. Add the apricots, if using.
- Dice the chicken into small pieces and toss in with the dressing.
- Serve with salad.
MAKES 4 SERVINGS
P.S. If you’re suffering from vaginal pain...
You need to try Julva – my restorative topical cream for the vulva. Its combination of DHEA and other high quality natural ingredients can help to relieve pain, repair skin elasticity, and stop external irritation of the vulva.
References (Part 2)
References (Part 1)
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3804006/
- .https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2815011/
- https://www.medscimonit.com/download/index/idArt/636058
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6390656/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5708798/#pone.0188812.ref020
- https://www.ncbi.nlm.nih.gov/pubmed/14747841
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3786579/
- https://obgyn.onlinelibrary.wiley.com/doi/pdf/10.1111/j.1600-0412.2011.01309.x
- https://www.hindawi.com/journals/mis/2018/5828071/abs/#B21
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4028155/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4625911
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3223258/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3804006
- Coffey, N, HERS Foundation Newsletter, Bayla Cynwyd, PA: HERS Foundation, Vol. V, Number 11.
- https://link.springer.com/article/10.1007/s00192-014-2490-y
- https://www.ncbi.nlm.nih.gov/pubmed/20362288
- https://www.medscape.com/viewarticle/805517_3
- https://www.ncbi.nlm.nih.gov/pubmed/17964350
- https://www.ncbi.nlm.nih.gov/pubmed/21850508
- https://www.ncbi.nlm.nih.gov/pubmed/10950229
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3804006/#R11
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2815011/
- https://insights.ovid.com/crossref?an=00042192-201805000-00006
- https://alumni.asu.edu/20181206-hysterectomy-linked-memory-deficit-animal-model
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3702015/