Several years ago I wrote a lengthy article on vaginal dryness solutions, along with treatments that were available for other women’s issues (incontinence, pelvic prolapse, low libido, pain during intercourse… just to name a few). You can read that article here
In that piece, I talked briefly about something called “vaginal rejuvenation”…
Vaginal what??!!!!
Have you heard that term being thrown about? If you have, you may have wondered what it is and if it might be something you should look into further.

So let me give you some basic information, from a physician (providing an OB/GYN’s point of view) who has focused on women’s health “down there” for decades.
First of all, “Vaginal Rejuvenation” isn’t really referring to a single thing anymore… it has become more of a marketing term that includes many different treatments including a variety of surgeries, laser procedures, injections, hormones and more.
And while vaginal rejuvenation originally focused on cosmetic surgeries and treatments to change the look and feel of the vagina (tightening a “loose” vagina and changing the size of the labias, primarily with the intent of improving sex and/or self-esteem... really, think of the original meaning to be more of a “facelift for the V!”), the term now encompasses so much more in the area of addressing true medical symptoms, referred to as “vaginal atrophy” symptoms, such as,
- Reducing vaginal dryness,
- Reducing pain during intercourse,
- Improving vaginal pH in order to reduce recurring infections
- Resolving incontinence (involuntary urinary leakage… that annoying peeing when you laugh, cough or sneeze!), pelvic prolapse (when your pelvic floor muscles weaken and organs literally start to fall downward!), and more.
But how do you know what might be relevant to your lady bits?
How do you know which solutions have research, physician endorsements and a track record of safety behind them, and more importantly, which don’t?
And now that the FDA has come out and issued warnings to 7 different companies offering some of these solutions… what does that mean? Is vaginal rejuvenation all just a bunch of hype?
Read on to find out more.
Vaginal Rejuvenation: Many Solutions, But What’s Right For You?
So not all vaginal rejuvenation solutions are equal! And while we want to stay away from those “facelift for the V” solutions, we may want to consider solutions that diminish our vaginal atrophy symptoms.
If you take a peek at my graphic you’ll see the differences relating to the invasiveness, cost, and controversy surrounding the various solutions found under the umbrella term, vaginal rejuvenation. In this article, I will be focusing a lot on laser therapy (as I get the most questions about this), but I did want to give you the broader overview as well.
Remember, always work with your medical practitioner to determine the best solutions for you, and always start with more non-invasive solutions first! Even if the non-invasive solutions don’t resolve all of your symptoms, they are at least improving the state of your vaginal tissue and muscle, which can only help if you try more invasive procedures later on.
On the “non-invasive” end of the spectrum, also the lowest cost and non-controversial solutions, you can find products such as lubricants and moisturizers (address vaginal dryness and pain, may improve libido since sex won’t hurt!), as well as pelvic floor strengthening exercises such as Kegels (addresses incontinence and pelvic floor health).
You also will find my Julva® women’s restorative cream for the vulva at this end of the spectrum (no prescription required; supports improvements in dryness, pain, leaking and pelvic floor health symptoms). I would definitely try this first, and yes, I am biased. These solutions provide a range of benefits relating to vaginal atrophy symptoms at relatively low cost and again, are non-invasive and even nurturing. Julva can also be used in conjunction with other therapies I will be discussing, including laser therapies, both prior to and after the procedure.
Further along the spectrum, you find hormone replacement therapies. Note that I only recommend the use of bio-identical hormones (if you aren’t sure what that is I have many blogs and Couch Talk podcasts on that topic). Bio-identical hormone replacement therapy requires medical supervision and a prescription but is proven to be effective at addressing many vaginal atrophy symptoms. Bio-identical hormone replacement therapy can also be used in conjunction with laser therapies.
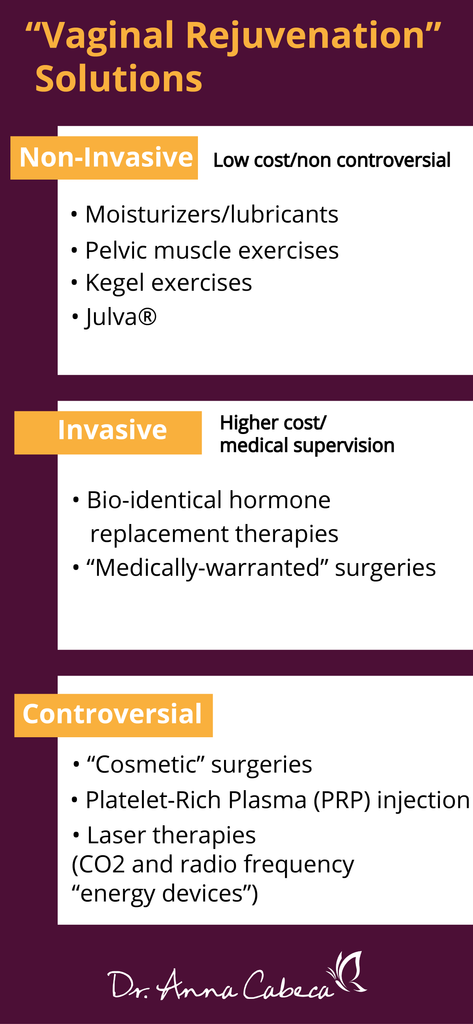
As you move across the spectrum towards more “invasive” solutions you’ll find laser treatments, PRP injections, and surgical interventions. The cost is higher as we move to the right, although some surgical interventions (those defined as medically-warranted) may be covered by insurance.
Note that cosmetic surgeries are considered controversial, and will not be covered by most insurance. Let’s talk briefly about these two categories of surgeries, then we’ll get into more details on laser therapies.

Medically-Warranted Surgeries
The two most common “medically warranted” vaginal rejuvenation surgeries – used to address prolapse and incontinence are uterosacral ligament suspension and sacrospinous ligament fixation. One that I favored from my Emory training with Dr.’s Cullen Richardson, MD and Bill Sayes, MD was the paravaginal repair where great care is taken to repair the broken fascia of the pelvic floor. Previous research published in 2014 reported that about 300,000 women in the US undergo surgery for prolapse every year. And that number is expected to grow, with about 44 million women dealing with symptoms of pelvic prolapse or pelvic floor problems by the year 2050!
I have performed these surgeries in the past and they can be very helpful for many women. I do not typically recommend them, however, without an initial focus on non-invasive approaches. Julva and Kegels, in particular, have shown great results in regards to supporting greater pelvic and vulvar health as well as prescribed vaginal testosterone and or DHEA. Note that these surgeries don’t address the issue of vaginal dryness, related pain during intercourse due to dryness, or diminished libido concerns.
Cosmetic Surgeries
I do not endorse cosmetic rejuvenation procedures with rare exception. These are really “plastic surgery” types of “designer” or “beautification”… really invasive procedures… to alter the labia minora and majora of the vagina (labiaplasty) or the folds of skin around the vulva (vaginoplasty) primarily for looks, versus medical necessity.
Note that I would consider for clients who had damage due to childbirth trauma, previous surgeries, wart removal, etc.

I always bring up orchids when talking to women about why they shouldn’t be ashamed or concerned if their vulva might look different than another. Just like the beautiful orchid – each unique in pattern and color – every woman’s vulva is completely unique and perfect for them.
Some women are tempted into surgery by comparing themselves to images they may see in porn; I say “No! Don’t do it!” (many of us refer to this anatomical perfection as the Barbie Doll vulva!) Unless the vulva is deformed in such a way that it inhibits either urinary or sexual function, or is associated with chronic discomfort, I say leave it be and embrace your uniqueness.
There are other surgeries that fall under the cosmetic category, including “revirgination” (hymenoplasty) surgeries that attempt to restore the hymen into a virgin state. Pleasssse! Just say no!
Note that the American Congress of Obstetricians and Gynecologists have questioned the safety and effectiveness of all of these cosmetic surgeries.
Laser Therapies – An Evolving Solution With The Great Promise
Near the middle of the spectrum for vaginal rejuvenation treatments, you will see a couple of different thermal laser therapies (CO2-based and something called Er: YAG-based) and also radio frequency-based laser treatments. There are numerous variations of these “energy-based” devices/treatments marketed by a multitude of providers. I’ll discuss a few here, along with some of the existing research.
First a few disclaimers!
Note that laser treatments are currently not FDA approved for the specific purposes of dryness, pain during intercourse, incontinence, pelvic prolapse, low libido or other symptoms that fall under the category of “vaginal atrophy”. The FDA had previously approved laser devices for “aesthetic use” and “gynecologic use”, but recently came out and clarified that their previous approval was not intended to apply to the treatment of these specific vaginal atrophy symptoms. Even without FDA approval, laser treatments are widely used to address such vaginal atrophy symptoms (as well as, unfortunately, being marketed for “facelifting the V!”). Physicians offer these treatments off-label frequently to address vaginal atrophy symptoms.
I’ll talk about this more, but many physicians, including myself, feel that laser therapies can be useful for patients presenting with vaginal atrophy symptoms, who have tried other less-invasive solutions (and where there are no other underlying medical conditions that should be treated).
There is research substantiating laser technology’s effectiveness when used appropriately. I do always recommend it be considered only under the guidance of an OB/GYN. That’s important, as you always want to ensure there isn’t something else going on that is causing the symptoms.
While I applaud the FDA for their concerns over women’s health and the potential for misuse (there are many providers out there without the appropriate medical knowledge who will gladly treat a woman for any number of vaginal rejuvenation services as if they were simply giving her a spa treatment!), I do feel they have gone overboard just a bit. There is a place for these treatments; in particular, I am talking about laser therapies, in helping women address major quality-of-life and health-affecting concerns.
The FDA shouldn’t limit a woman’s right to make an informed choice about their vagina!
I really do feel that the issue the FDA is hyper-focusing on is the “cosmetic” piece of these treatments. Getting laser therapy for cosmetic reasons, versus medical symptoms, is a valid concern. Not all lasers are alike, and I worry that women getting treatments in “health spas” could be potentially harmed by the use of fewer quality lasers, the lack of a qualified medical professional and/or having such treatments in lieu of other needed medical care.

OK, so now onto the info! How do lasers work and what has the research shown?
So, how does laser therapy work?
I’m going to focus more on CO2 lasers versus Er: YAG or radio-frequency lasers as I am most familiar with the research relating to CO2. But they all are very similar in practice.
For some time, CO2 lasers have been widely used in plastic surgery and dermatology and have proved to be both beneficial and safe for tissue remodeling around the face and neck. The laser energy that is emitted by such lasers is absorbed by water in the tissue that is being treated. The heat generates thermal micro millimeter tissue damage, causing ablation (destruction) of the tissue. It is actually then the wound-healing process that is triggered by this targeted damage that results in the beneficial results to the tissue.
CO2 lasers like the Mona Lisa Touch are considered fractional lasers. Much of the existing research has been done using fractional lasers. The fractional approach simply means that the thermal energy is delivered in a fractional pattern. This is important as the healthy tissue is left surrounding each ablation area, in a pattern, which helps support more rapid epithelial repair and collagen production (and elastin fiber formation that provides the firmer and tighter tissue, reducing the “looseness” or “laxity” of the vagina). Fractional CO2 laser treatments have been shown to improve vaginal atrophy symptoms, and biopsies show that the vaginal wall epithelium is thicker and healthier (actually resembling a non-atrophied vaginal state). This means more natural lubrication and elasticity.
CO2 laser therapy is a simple procedure taking 5-20 minutes. It involves introducing the laser device into the vagina with the practitioner rotating it and slowly withdrawing it. Usually, only a few treatments are required at intervals of 4-6 weeks, and results may last as much as a year. Then a patient may need to have another treatment. It isn’t painful… well, except perhaps for the cost. A series of treatments can run up to 3K and is not typically covered by insurance.
The Research Behind Laser Vaginal Rejuvenation
There have been a number of studies relating to the use of lasers in both perimenopause and postmenopausal women with clinical symptoms of vaginal atrophy. This again includes symptoms of dryness, weakened and thinning vaginal walls, discomfort during intercourse, pelvic prolapse, urinary incontinence, and loss of libido.
So why, you might ask, are people concerned about laser therapy is given there is existing research that has shown it to be safe and effective?
Well, as with a lot of research, more data is still needed, such as information from long-term follow-up studies. More randomized trials and comparative studies also need to be published and the specifics relating to the ideal “dosage” (length of individual treatments, number of treatments, temperature, etc.) need to be assessed.
Although the initial studies indicate the laser treatments are effective and appear to be safe, further studies would help assess things such as whether other proximal organs (urethra, bladder, rectum) could be affected. The FDA has also stated they’ve received reports relating to women having burns, pain and other ill-effects (although this general statement hasn’t been tied to any given device, procedure or provider).
I believe the real issue behind the FDA’s recent statement isn’t the procedure so much as it is the “Wild West” mentality of many clinics out there that are treating it like a spa treatment versus a medical procedure. Ladies, it is a medical procedure, not a Brazilian wax; so it is important to talk with your physician about your particular set of concerns.
Now let’s talk a bit about some of the research.
For fractional CO2 lasers, there have been a variety of studies done focused on vaginal atrophy symptoms.
In the first study, I’ll mention, 386 menopausal women with vaginal atrophy symptoms were treated with just three treatments of a fractional CO2 laser. After three treatments, patients reported improvement of symptoms (59.94% dryness, 56.26% burn, 73.15% soreness, 48.75% dyspareunia, 56.37% itch and 48.79% pain). Even after just the first session, there were beneficial effects; and beneficial effects were confirmed one year after the last session.
In another study using a fractional CO2 laser, the focus was on vaginal atrophy symptoms as well as on sexual function and satisfaction in 77 post-menopausal women with vaginal atrophy symptoms. Significant improvements were found across all measures: lubrication, pain, desire, arousal, orgasm, and satisfaction. Another finding was that 85% of a smaller group of 20 women, not sexually active prior to the treatment due to the severity of vaginal atrophy symptoms, regained a normal sexual life at the 12-week follow-up.
In a more recent study, 28 post-menopausal women with vaginal atrophy symptoms were treated with fractional CO2 laser. One month after the initial treatment there was a significant improvement in symptoms. A further significant improvement was seen at 3 and 6 months following the third laser treatment.
Stress Urinary Incontinence (SUI) has been studied using laser therapies as well. In one study, 175 women of various ages, diagnosed with SUI were treated with Er: YAG laser therapy with 77% having a significant improvement in SUI symptoms.
An interesting review of available research was done in 2017 that shows that laser therapy works. The results of multiple studies have all been positive, with the therapies penetrating the vaginal wall to stimulate ablation, which in turn improves collagen synthesis and natural lubrication of the vaginal wall.
The author summary in this review paper stated:
“A consensus has been reached among the authors of this manuscript on the clinical effectiveness of energy-based therapies on GSM-related symptoms (Genitourinary Syndrome of Menopause, another term for vaginal atrophy, urogenital atrophy, or atrophic vaginitis). The currently available data on the effects of fractional laser and RF on the skin, and additional information reported in almost 20 peer-reviewed publications on GSM-related symptoms, unequivocally demonstrate the following changes: thickening of glycogen enriched postmenopausal epithelium, neovascularization, and neocollagenesis in the lamina propria, increased lactobacilli counts, reduced pH, vaginal wall tightening, and improved urination control with minimal risk of short- and long-term complications.”
Today, even after the FDA clarification on their views, you can find a wide variety of respected hospitals and medical institutions who offer these services. Johns Hopkins and Northwestern just to name two.
Many of my peers routinely recommend laser therapies to their patients to address medical symptoms. I’m honored that they also recommend Julva as part of pre and post-treatment care.
Beyond CO2 Lasers
I wanted to briefly mention a few other laser therapies. Beyond CO2, another type of ablative laser being utilized is the Er: YAG laser which emits laser energy in the mid-infrared invisible light spectrum. This means it has 10 to 15 times the affinity for water absorption compared with the CO2 wavelength. There are a number of clinical studies that have shown the Er: YAG to also be effective for vaginal atrophy and SUI symptoms. I won’t go into them all here, but you can do a few searches if interested, lots of PUBMED references online for free. Here is one study done with the Fotona laser.
It is worth mentioning that an international multicenter observational study is currently underway to evaluate the efficacy and safety of Er: YAG laser for the treatment of genitourinary syndrome and stress urinary incontinence, called VELAS, the Vaginal Erbium Laser Academy Study. This study will evaluate the effects of three Er: YAG laser applications when used across 1,500 postmenopausal women. The women will be followed for one year. Perhaps the results of this study will help sway the FDA relating to laser’s effectiveness for addressing vaginal atrophy symptoms.
One other type of laser you may read about is radio frequency lasers. There also have been studies showing that they can help with vaginal atrophy symptoms. Again, there are many free studies online.
Now let’s go back and look at our spectrum of solutions.
There are a few others to talk about.
Platelet-Rich Plasma Injections
One that I have recommended to some clients in the past is Platelet-Rich Plasma (PRP) injections.
In this procedure, your own blood is drawn and the platelet-rich plasma is removed. This plasma, rich in your own growth factors, is then injected into tissue to stimulate regeneration and repair. Physicians have used PRP in areas around the urethra, labia, clitoris, and G-spot to improve tissue health, tone and sensitivity. The procedure is used elsewhere, such as in dentistry, orthopedics and skin care, as well.
The G-spot is an area on the anterior wall of the vagina and has been documented as an area of increased orgasmic sensitivity. It has been a controversial topic, with the American College of Obstetricians and Gynecologists including G-spot injections in their 2007 position paper condemning cosmetic-focused vaginal rejuvenation surgeries and procedures. The treatment is sometimes referred to as “O-spot” treatment (O being orgasm).
There have been multiple studies showing it to be safe and effective in areas such as wound care, sports medicine, dental surgery, orthopedics, and more. And there is one pilot study that has shown PRP may be safe and effective for improving sexual function.
I used collagen with patients over the years for G-spot injections prior to PRP coming out. I had good results with G-Spot injections in achieving sexual function improvements in many patients.
PRP has also emerged as a means to improve grafting related to treating vaginal atrophy and a condition called lichen sclerosus. In this procedure PRP and hyaluronic acid have been injected in the perineum area as a part of lipofilling (a reconstructive technique using fat grafting to reconstruct the vaginal walls, originally used with vaginal wall defects) and the results of this lipofilling have been to restore the fullness of the labia as well as achieve remission of lichen sclerosus on the labia minora.
This is similar to research using lasers to build up the vaginal wall, specifically to build up vaginal rogation (folds). Decreased rugae appear to be related to other vaginal atrophy symptoms appearing in advanced age and reduced estrogenic levels. The CO2 laser has been used to increase rugae, increase sensation and improve sexual function in women.
Finally, another vaginal rejuvenation procedure is using biocompatible material to address vaginal laxity by building up the vaginal walls. In this procedure, Gore-Mycromesh was inserted under the submucosa of the vaginal wall. Results found a substantial improvement to sexual function a year after surgery.
With concerns for mesh erosions, I highly recommend using Julva pre and post and prescribed vaginal androgen hormones.
I created Julva, a restorative topical cream for the vulva for this very reason. It has helped thousands of my patients (as well as myself) experience significant symptom relief and feel good about their sexual health again. My focus when creating Julva was to make sure that it heals long-term, and that it’s safe for the female body (it's also safe for the men who may get it on them!). It had to have anti-aging benefits, had to be easy to use, and had to smell and feel good. The most important thing was that it had to be all-natural, with no additives or toxins.
And that is what Julva is all about, all-natural. Along with DHEA, it contains alpine rose plant stem cells, vitamin E, coconut oil, emu oil and shea butter.
>>> Click the link below for your free 7-day trial pack<<<
It is exciting for me, after so many years focused on women’s health and the health of their “Vs” to see well-researched procedures used for years in other medical areas now being applied to improve women’s lives.
Final Words On Vaginal Rejuvenation
I hope this info helps you in understanding a little about the various treatments that are available to address vaginal atrophy symptoms and which ones are supported by both the research and many of us in the medical community.
It is important to me to provide as much research to my community as possible so that women can make an informed choice about their bodies!
And yes, by addressing vaginal atrophy symptoms you will likely improve sexual function and even satisfaction but…
Please don’t even consider invasive procedures for purely cosmetic reasons… or because you think “looking better down there” will somehow improve sex. You are beautiful and sexy just as you are. Remember the orchid!
Try the least invasive solutions first, and work with a practitioner, preferably an OB/GYN to evaluate other “vainal rejuvenation” treatment options should you still have symptoms. You want to be sure you fully understand your particular symptoms and whether you have underlying conditions that should be treated in a different manner.
Whether those symptoms be due to hormone decline due to aging, diminished pelvic health after childbirth, you need to find a non-estrogen solution due to cancer concerns, whatever… please consider undertaking these more invasive treatments for medical reasons only. No more focus on Barbie-Doll vulvas!
Now excuse me while I go have some tea while I take a beautiful soak with my favorite “V-friendly” essential oils (tea tree oil and chamomile, don’t forget to use a carrier oil!)... followed by Julva, of course!





