Understanding the cortisol-metabolism connection and evidence-based strategies for hormonal recovery
In This Article, You Will Learn:
• How chronic stress triggers cortisol imbalances that disrupt metabolism
• The specific ways stress hormones affect weight, energy, and overall health in women
• Science-backed nutritional and lifestyle interventions for stress recovery
• How targeted supplementation can support healthy cortisol rhythms
• Practical strategies to break the stress-weight gain cycle
If you've been struggling with unexplained weight gain, energy crashes, or feeling like your body just isn't responding the way it used to, you're not alone. What many women don't realize is that chronic stress may be the hidden culprit behind these frustrating symptoms — and it all comes down to your hormones.
Recent research has revealed a complex web of connections between our stress response system and metabolic function, particularly in women over 40. When we understand these mechanisms, we can finally address the root cause rather than just managing symptoms.

Your body's stress response system, known as the hypothalamic-pituitary-adrenal (HPA) axis, was designed to help you survive immediate threats. When you encounter stress, your adrenal glands release cortisol — often called the "stress hormone" — which triggers a cascade of physiological changes.
In acute situations, this system works beautifully. Cortisol increases blood sugar for quick energy, heightens alertness, and temporarily suppresses non-essential functions like digestion and reproduction. The problem arises when this emergency response becomes chronic.
Dr. Robert Sapolsky's groundbreaking research, published in Endocrine Reviews, demonstrates that chronic cortisol elevation leads to metabolic dysfunction, insulin resistance, and increased abdominal fat storage¹. For women navigating perimenopause and menopause, this becomes even more complex as declining estrogen levels can amplify cortisol's effects.
The Cortisol-Metabolism Connection
When cortisol remains elevated for extended periods, several metabolic disruptions occur:
Insulin Resistance Development: Chronic cortisol exposure makes your cells less responsive to insulin, leading to higher blood sugar levels and increased fat storage, particularly around the midsection.
Appetite Dysregulation: Elevated cortisol triggers cravings for high-calorie, high-carbohydrate foods. This isn't a willpower issue — it's your body's biological drive to store energy for perceived ongoing threats.
Muscle Mass Reduction: Prolonged cortisol elevation can break down muscle tissue for glucose production, lowering your metabolic rate and making weight management increasingly difficult.
Sleep Disruption: Cortisol naturally follows a circadian rhythm, peaking in the morning and declining throughout the day. Chronic stress disrupts this pattern, often causing elevated evening cortisol that interferes with sleep — creating a vicious cycle since poor sleep further elevates stress hormones.

Women face unique challenges when it comes to stress hormone balance. The intricate dance between cortisol, estrogen, progesterone, and other hormones becomes increasingly complex during perimenopause and menopause.
Research published in Psychoneuroendocrinology shows that women have more reactive stress response systems than men, with greater cortisol release in response to psychological stressors². Additionally, the decline in estrogen that occurs during midlife removes a natural buffer against cortisol's effects.
The Perfect Storm of Modern Life
Consider the multiple stressors facing today's women:
Career demands and workplace pressure
Caregiving responsibilities for children and aging parents
Financial concerns and planning for the future
Health concerns and body changes during midlife
Information overload and social media pressure
Sleep deprivation and busy schedules
Each of these stressors triggers cortisol release. When they occur simultaneously and persistently, your stress response system becomes overloaded and dysregulated.

The good news is that stress hormone imbalances are not permanent. With targeted interventions, you can restore healthy cortisol rhythms and metabolic function. Here's what the research shows works:
Nutritional Strategies for Cortisol Balance
Stabilize Blood Sugar: Fluctuating blood glucose levels trigger cortisol release. Focus on balanced meals combining protein, healthy fats, and complex carbohydrates. Avoid skipping meals, which can spike cortisol levels.
Support Adrenal Function: Certain nutrients are particularly important for healthy stress response:
Vitamin C: Acts as a cofactor in cortisol synthesis and helps moderate excessive production
B-complex vitamins: Essential for neurotransmitter production and stress resilience
Magnesium: Helps regulate the HPA axis and promotes relaxation
Omega-3 fatty acids: Anti-inflammatory and help modulate cortisol production
Consider Adaptogenic Support: Adaptogenic herbs have been shown to help normalize cortisol levels and improve stress resilience. Research on specific adaptogens like ashwagandha, rhodiola, and holy basil demonstrates their ability to modulate the HPA axis³.
For women seeking comprehensive adrenal support, Mighty Maca® Plus provides a carefully formulated blend of adaptogens, vitamins, and minerals specifically designed to support a healthy stress response. This powerful superfood blend includes maca root, which has been traditionally used to support hormonal balance and energy levels.
Lifestyle Interventions That Work
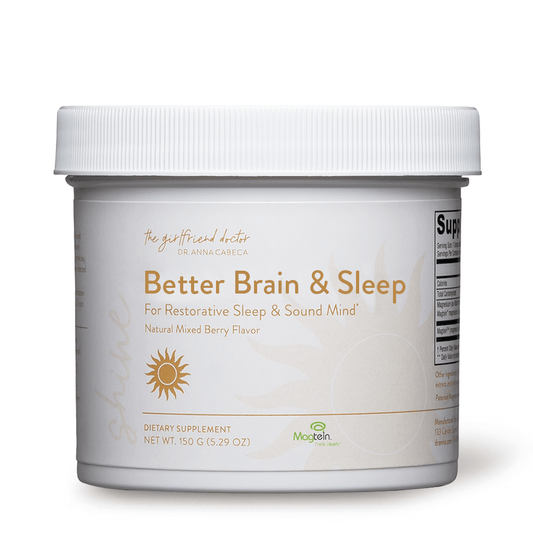
Prioritize Sleep Hygiene: Quality sleep is essential for cortisol regulation. Establish consistent sleep and wake times, create a cool, dark sleeping environment, and avoid screens for at least an hour before bed.
Practice Stress-Reduction Techniques: Regular meditation, deep breathing exercises, or yoga can significantly reduce cortisol levels. Even 10 minutes of daily practice can make a measurable difference.
Exercise Strategically: While exercise is crucial for health, excessive high-intensity training can elevate cortisol. Focus on moderate-intensity activities like walking, swimming, or gentle strength training, especially if you're already dealing with high stress levels.
Build Social Connections: Strong social support networks have been shown to buffer against stress and reduce cortisol production. Prioritize relationships and community connections.
Targeted Supplementation for Hormonal Balance
For women experiencing significant stress-related symptoms, targeted nutritional support can be transformative. Balance offers a unique approach to hormonal support, providing bioidentical progesterone in a topical cream that bypasses digestive processing for optimal absorption.
Progesterone acts as a natural anti-anxiety agent and can help counterbalance cortisol's effects. Many women notice improved sleep, reduced anxiety, and better mood stability when progesterone levels are optimized.
Additionally, Keto-Green® Detox provides comprehensive support for the body's natural detoxification processes, which can become overwhelmed during periods of chronic stress. This carefully formulated supplement helps support liver function and cellular detoxification pathways.
The Gut-Stress Connection
Emerging research reveals a bidirectional relationship between gut health and stress hormones. Chronic stress can disrupt the gut microbiome, while an imbalanced microbiome can trigger inflammatory responses that elevate cortisol.
Supporting digestive health through probiotic-rich foods, prebiotic fiber, and stress-reduction techniques can help break this cycle. Consider working with a healthcare provider to assess gut health if you're experiencing persistent digestive issues alongside stress symptoms.
Real Women, Real Results
The power of addressing stress-hormone imbalances goes beyond just the science — it's about real women reclaiming their health and vitality.
Sarah, a 48-year-old executive, shared: "I thought my constant fatigue and weight gain were just part of getting older. Once I started addressing my stress levels and supporting my adrenals nutritionally, I felt like myself again. My energy returned, and the weight started coming off naturally."
Maria, age 52, reported: "The brain fog was the worst part. I couldn't think clearly, and I was so frustrated. Learning about the cortisol connection and implementing stress-management strategies changed everything. I feel sharp and focused again."
These experiences reflect what research consistently shows: when we address the root cause of hormonal imbalances rather than just managing symptoms, profound healing becomes possible.

The Path Forward: Sustainable Stress Management
The relationship between stress hormones and metabolism is complex, but understanding these connections empowers you to take targeted action. By addressing chronic stress through evidence-based nutritional, lifestyle, and supplementation strategies, you can restore hormonal balance and metabolic function.
The key is consistency and patience. Your body's stress response system didn't become imbalanced overnight, and healing takes time. But with the right approach, you can break free from the stress-weight cycle and reclaim your energy, mental clarity, and overall well-being.
If you're ready to address the root causes of your symptoms rather than just managing them, consider working with a healthcare provider who understands the complex interplay between stress, hormones, and metabolism. Your health journey is unique, and personalized support can make all the difference.

Q: How long does it take to see improvements in cortisol levels with lifestyle changes?
A: Most women begin noticing improvements in energy and sleep within 2-4 weeks of implementing consistent stress-management strategies. Measurable changes in cortisol levels typically occur within 6-12 weeks of sustained intervention.
Q: Can stress really cause weight gain even if I'm eating well and exercising?
A: Yes, chronic stress can cause weight gain independent of caloric intake through several mechanisms: increased cortisol promotes fat storage (especially abdominal fat), disrupts insulin sensitivity, and can slow metabolic rate by breaking down muscle tissue.
Q: Are adaptogenic supplements safe to take long-term?
A: Most adaptogenic herbs are considered safe for long-term use when taken appropriately. However, it's best to work with a healthcare provider to determine the right approach for your individual situation, especially if you're taking medications or have underlying health conditions.
Q: What's the difference between acute stress and chronic stress in terms of health effects?
A: Acute stress is short-term and can actually be beneficial, improving performance and immune function. Chronic stress occurs when your stress response system remains activated for extended periods, leading to hormonal imbalances, metabolic dysfunction, and increased disease risk.
- ¹ Sapolsky, R.M. (2000). Stress hormones: good and bad. Endocrine Reviews, 21(3), 237-267.
- ² Kajantie, E., & Phillips, D.I. (2006). The effects of sex and hormonal status on the physiological response to acute psychosocial stress. Psychoneuroendocrinology, 31(2), 151-178.
- ³ Chandrasekhar, K., Kapoor, J., & Anishetty, S. (2012). A prospective, randomized, double-blind, placebo-controlled study of the safety and efficacy of a high-concentration full-spectrum extract of ashwagandha root in reducing stress and anxiety in adults. Indian Journal of Medical Research, 136(4), 637-645.